PSG Hospitals’ maiden foray into specialties began on November 3, 1994, when the Department of Cardiology started functioning. The then fledgling department had just the basic facilities.
Over the next two decades, a large number of major procedures have been added, including pacemaker implantation, balloon angioplasty and stenting, with state-of-the-art equipment at its disposal. This is a veritable testimony to the department’s growth.
Initially it was a three-member team headed by Dr J.S.Bhuvaneswaran. The department is currently headed by
Dr G. Rajendiran, and has expanded with six consultants supported by specialised technicians and nursing staff.
An emergency ambulance, fully equipped for acute coronary care is available. The department offers round-the-clock, nine-bedded Intensive Coronary Care.
The electrophysiology lab, established in July 2012, facilitates mapping of the heart’s electrical activity and thus helps doctors to zero in on the cause or source of abnormal heartbeats. The department began offering superspeciality course in cardiology since 2010, as academic and research activities are quintessential for any health care facility to raise the bar of patient care. Specialised technical training in intensive care and diagnostics is also provided by the department.
The department believes in protocols and standardization of treatment .We have written protocols for both common and uncommon disease entities so that there is completeness and uniformity in treatment .This also should make publications easy in coming years.
Education of patients is our strength. We have an exclusive preventive department team and clinical nurse who are involved in educating patients. A team consisting of a rehabilitation expert, a dietician, a cardiac counsellor and a yoga therapist is involved under a Cardiologist’s supervision. We have formed a library exclusively for patients to read and learn . We also have installed a television to spread information. Booklets on common diseases are available both in tamil and English for patients to learn about their problems and drugs .
The preventive team visits our sister institutions and other institutions to educate people and screen them for risk factors.
The team aims to focus on young MI patients. Apart from offering them complete rehabilitation measures , we have initiated few studies as our research projects focusing on etiopathogenesis of atherosclerosis in the young.
Clinical Auditing adds to our quality of work
It is our pride to inform you that The Department of Cardiology and Angiology,PSG IMS&R is involved in dedicated cardiac and peripheral interventions for the past two decades. We have a fully equipped coronary care unit, State of the art cath lab with consultants available round the clock for emergency services.
Download PDF BrochureCardiac Electrophysiology is one of the fastest progressing fields in modern medicine. Cardiac Electrophysiology (EP) is the study of the heart’s electrical activity; aimed at analysing, diagnosing, and treating its electrical disorders.
Cardiac EP procedure studies this phenomena by recording the electrical activity of the heart using multiple invasive catheters. These studies also help in diagnosing complex Heart Rhythm Disorders. These procedures include therapeutic methods (typically RF Ablation) along with other diagnostic and prognostic procedures. Cardiac EP also includes antiarrhythmic drug therapy, implantation of pacemakers and Implantable Cardioverter- Defibrillators (ICDs) and Cardiac resynchronisation therapy devices or COMBO devices for heart failure management and prevention of sudden cardiac death.
Cardiac electrophysiologists perform interventional cardiac Electrophysiology Studies (EPS) and surgical device implantations. PSG hospitals are among the very few cardiac centres in south India with state-of-the-art advanced St Judes precision velocity 3D mapping system. The EnSite Velocity™ 3D Cardiac Mapping System is a non-fluoroscopic mapping and catheter navigation system. The System creates three dimensional (3D) models that are based on the anatomy of the patient’s own cardiac chamber. Cardiac electrical activity can be displayed as waveform traces or as dynamic activation or voltage maps which are superimposed on the 3D models. The navigation system displays the real time position of conventional electrophysiology catheters in relation to the 3D model. The EnSite Velocity System has been designed for ease-of use and helping in mapping all complex arrhythmias and help in curing these difficult arrhythmias.
- Electrophysiology study for all Heart Rhythm Disorders
- Radio frequency ablation for common Tachycardia (e.g. Supra-Ventricular Tachycardia)
- Radio frequency ablation for complex Tachycardia (Atrial fibrillation, Atrial Flutters, Ventricular Tachycardia) using state of art 3-D mapping and ablation system.
- EP study and RFA in paediatric Tachyarrhythmias.
- Cardiac device implantation (permanent pacemakers, ICDs)
- ICDs for prevention of sudden cardiac death.
- LAA (Left Atrial Appendage) closure for Atrial Fibrillation
- Leadless pacemaker insertion for bradycardia with heart blocks.
- Implantable loop recorder, external loop recorder, Head up Tilt testing,Holter monitoring for short and long-term heart rhythm monitoring purposes.
- Speciality clinics for Syncope evaluation which includes Head Up Tilt Table testing for vasovagal syncope and evaluation of orthostatic intolerance including cardiac autonomic testing.
- Head up tilt table test( HUTT)
Heart Failure (HF)
Heart failure is a disease sometimes known as congestive heart failure, occurs when your heart muscle is not able to pump blood as well as it should. The prevalence of HF is approximately 1–2% of the adult population, rising to ≥10% among people more than 70 years of age. Among people more than 65 years of age presenting to primary care with breathlessness on exertion, one in six will have unrecognized HF
Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or stiff to fill and pump efficiently. Basically, the heart can’t keep up with its workload.
HF may require repeated hospitalization, advanced investigations and advanced treatment options. A multidisciplinary team (MDT) approach is considered the gold standard model for the delivery of HF care.
Our Team Consists of
A Dedicated Cardiologist trained in Advanced Heart Failure & Heart Transplantation and an Electro physiologist. Heart failure trained clinical pharmacist, to educate you about your medications, adjust your medications, monitors and prevents adverse drug reactions.Trained Physiotherapists, who ensures effective rehabilitation of patients with Heart failure to improve quality of life. Trained Heart failure staff nurses, to ensures effective patient care. Trained dietian, who tailors salt and fluid prescriptions according to the clinical situations and reinforce whenever clinically indicated.
Heart Failure Rehabilitaton Centre
Cardiac rehab is a medically supervised program that includes exercise training, education on heart-healthy living, and in many cases, counseling to reduce stress. It helps patients recover and improve physical, mental and social function. The goal is to stabilize, slow or even reverse the progression of heart failure. This can help reduce the risk of heart disease,another cardiac event or death. This is one of the very few centers in India and first of its kind in Tamilnadu where a structured cardiac rehabilitation services are available with advanced equipments. It is equipped with CPET, motorized treadmills, Elliptical trainer and Recumbent cycle to provide personalized rehabilitation service.
CPET (Cardiopulmonary Exercise Testing)
Cardiopulmonary system is assessed during a CPET by measuring the amount of oxygen your body is using, the amount of carbon dioxide it is producing, your breathing pattern, and electrocardiogram (EKG) while you are riding a stationary bicycle. It is an advanced form of exercise testing, helps in tailoring the exercise prescription and also guides the treating physician regarding advanced therapies in Heart failure.
Six Minute Walk Test
We assess walking distance covered in 6 minutes with careful monitoring of symptoms,vital signs, which helps the treating physician in making treatment decisions.
Heart Failure Counseling
Our trained clinical pharmacist and clinical nurse specialists counsel the patients, so that they understand their illness, medications and treatment options for the patients during their hospital stay.
Training in Self-management
Patients are encouraged and trained in self-management, which included monitoring weight, urine output and adjusting the dosage of water pills ( diuretics ) accordingly. This improves the quality of life and decreases the rate of readmissions. Patients are advised to monitor for set of symptoms which helps them to identify decompensations early so that it can be acted upon.
Guideline Directed Medical Therapy
Our team ensures optimization of medications which is essential for optimal outcome along with careful monitoring for adverse drug reactions.
Ambulatory Inotropic Therapy
It is used in selected patients with end-stage heart failure who are inotrope dependent can be treated at home while awaiting other definitive therapies.
Cardiac Resynchronization Therapy and Implantable Cardioverter Defibrillator Implantation
Cardiac resynchronization therapy is a procedure to implant a device in your chest to make your heart’s chambers contract in a more organized and efficient way. The signals tell your ventricles to contract at the same time, maximizing the amount of blood that’s pumped out of your heart. These are high-end implantable devices that help the heart to improve its efficiency and also regulate its rate. They are life-saving in many of situations.
An implantable cardioverter-defibrillator or automated implantable cardioverter-defibrillator is a device implantable inside the body, able to perform cardioversion, defibrillation, and pacing of the heart. The device is therefore capable of correcting most life-threatening cardiac arrhythmias
Heart Transplantation
Our journey of organ transplantation started in 1998 when we started the renal transplantation program and now we have successfully performed 330 renal transplants so far. We successfully conducted our first Liver transplantation in 2012 Our Liver transplant team is regularly involved in cadaveric as well as living donor liver transplantation and now we have performed 50 Liver transplants so far. We have started our lung transplantation program in 2017 and is being the first teaching hospital in India to perform a successful sequential double lung transplantation procedure.
Heart transplantation is a surgical transplant procedure being performed on patients with end-stage heart failure, severe coronary artery disease or complex congenital heart diseases when other medical or surgical treatments have failed. Though this is an established method of treatment and is being performed routinely in western countries, it is being performed in routinely India only for the past one decade. PSG SSH is well equipped and geared up to start its heart transplant program.
Paediatric Cardiology is a subspeciality which deals with children affected with heart diseases. We all know that “a child is not a small adult”. Children are in the growing phase of their life. Their body size, body functions, drug dosages and treatment of heart diseases are all different depending on their age, weight and phase of development. Hence it becomes necessary for a clinician with knowledge of cardiology and paediatrics to treat such diseases – a paediatric cardiologist. Diseases affecting children may be congenital or acquired. Congenital heart diseases are heart defects present from birth. They are of many types – shunt lesions (holes in the heart), valvar stenosis (blockages in the valves) and complex cyanotic heart diseases (combinations of the above which lead to low oxygen levels). Acquired heart diseases broadly include diseases which develop after birth. They include infections of the heart, heart failure and abnormal rhythms in the heart.
GUCH basically means “grown up with congenital heart disease”. Some congenital heart diseases which are undiagnosed during childhood may manifest themselves only in adulthood. These are treated by cardiologists with a knowledge of congenital heart disease.
Treatment for both congenital and acquired heart diseases vary from watchful waiting , medications to interventions and open heart surgery depending on the condition of the patient and type of disease. PSG superspeciality hospitals is well equipped with paediatric and adult cardiologists to treat all such diseases.
The following facilities are available in the Department of Paediatric Cardiology and GUCH:
- 1. ECG and Chest X-ray
- 2. Treadmill Test
- 3. Ambulatory Blood Pressure monitoring for Paediatric and Adult Patients
- 4. State of the art Transthoracic and Trans esophageal 2D and 3D echocardiography to diagnose all types of acquired and congenital heart defects.
- 5. State of the art cardiac catheterisation labs to perform all types of diagnostic and interventional procedures for congenital heart diseases.
- 6. Some of the procedures performed include
- Diagnostic right and left heart cardiac catheterization.
- Pretransplant Cardiac Catheterisation.
- Endomyocardial biopsy.
- Neonatal, Paediatric and Adult balloon valvuloplasties.
- Device closures of all intracardiac shunts.
- Complex Neonatal PDA and RVOT stenting.
- Coarctation and Branch Pulmonary artery stenting.
- Percutaneous Pulmonary Valve Implantation.
- EP study and RF ablation for Paediatric and GUCH arrhythmias.
- 7. Paediatric Heart failure clinic. Heart failure is generally a condition where the heart is not strong enough to pump blood to the body. Such patients need various types of treatment including intensive heart medications, Ventricular Assist Devices and Heart Transplantation. The Paediatric Heart Failure clinic is well equipped to deal with such patients starting from diagnosis, work up and treatment upto heart transplantation and its future care.
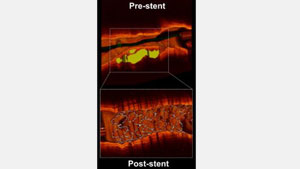
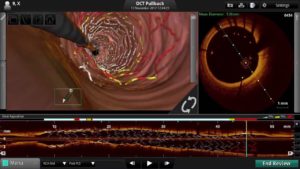
Center Of Excellence For Coronary Imaging
3D OCT an advanced imaging technology has been launched at PSG hospital fully integrated with Cath lab first of its kind in Coimbatore.
This technique uses catheter-based equipment with infrared light to acquire 3D images of a blood vessel supplying the heart. The image resolution is 10 times higher than ultrasound.
The primary advantage of OCT is to optimize the angioplasty procedure(Stent implantation ) so as to ensure ultimate long term results and identity complications.OCT images can clearly show calcium, fat, blood clots inside the coronary arteries, nature of in stent re stenosis(Reblockages after stent implantation).
Centre For Advanced Transcatheter Valve Interventions
What is transcatheter valve replacement?
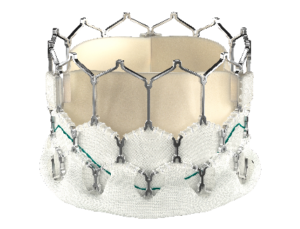
Transcatheter aortic valve replacement (TAVR/TAVI) is a treatment option for some patients with severe aortic stenosis (narrowing of the aortic valve opening). TAVR/TAVI is less invasive than traditional surgery. The procedure itself takes only about an hour without the need for open-heart surgery.
Who can have TAVI?
If you have been diagnosed with severe aortic stenosis and your doctor has evaluated the same, TAVR/TAVI may be a better alternative for you. A specialized Heart Team involving an Interventional Cardiologist and a cardiothoracic surgeon can determine which treatment option is best for you.(TAVI or Surgical AVR)
Your doctor would need to evaluate and plan for your TAVR/TAVI case by conducting a few medical and clinical tests like Echocardiogram, CT scan, most of which can be done as an outpatient.
TAVI Approaches
There are several ways to implant the new valve. Your doctor will decide which approach is the best for you and may mention approaches other than those described below.
- The transfemoral approach (the most common approach and is through the thigh).
- The subclavian approach (through an incision near the shoulder).
- The transapical approach (through an incision in the chest between the ribs).
- The transaortic approach (through an incision in the upper chest).
How is the Procedure Done
Your aortic valve will be replaced with a valve made from tissue (biological). The tissue is supported with a metal frame. Despite the metal frame, having the valve will not require you to take blood thinners. But, if you are already taking a blood thinner, you will need to keep taking it.
- The thigh area(Femoral artery) is numbed, and either a local anaesthetic with sedation or a general anaesthetic is given.
- The balloon catheter is guided into your heart and positioned within the opening of the aortic valve
- The doctor implants a new aortic valve using a metal mesh tube which keeps the valve in place – the new valve either expands by itself or is expanded using the balloon, depending on the type of valve used.
- The new valve is positioned to push aside your damaged aortic valve.
- The balloon is deflated and your doctor removes the balloon then the new Valve will start functioning immediately.
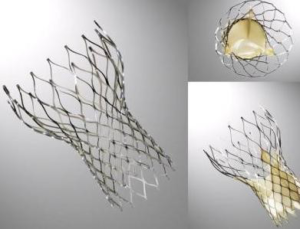
Types of TAVI valves?
Self-Expandable THV & Balloon Expandable THV
Valve in Valve TAVI
Patients who had SAVR or surgical mitral valve replacement may develop valve degeneration in 10 to 20 years after surgery can opt for “valve- in- valve” (ViV) procedure. A valve-in-valve TAVI procedure involves placing the new valve (aortic or mitral or tricuspid or pulmonic) into the old one using a transcatheter approach. You may be able to have a valve-in-valve procedure if:
- Your old valve was replaced with a prior bioprosthetic valve
- Your old valve opening is the right size to support a transcatheter valve
- You are considered high risk for traditional heart surgery
- You don’t have other valve conditions that would be best corrected with traditional heart surgery.
Follow-up care
Post procedure usually patients are discharged within 2 -3 days. You will need to visit your cardiologist one week after the procedure and then visit within one month during initial review
Centre For Complex Coronary Interventions
Our center has been routinely performing complex coronary interventions with the aid of advanced hardwares
- Image guided interventions-IVUS/OCT
- Coronary Physiology-Fractional Flow reserve(FFR/RFR)
- Chronic total occlusion (Long standing 100% blockages) via antegrade and retrograde approaches
- Left main and bifurcation PCI
- Graft interventions
- Rotablation guided PCI/Shock wave lithotripsy
An Initiative Towards Healthy Living
Heart Diseases continue to be one of the leading causes of death in India. There is also a recent uprise of heart diseases in younger age group, thus contributing to a huge social and economic burden. We keep hearing about the loss of famous film personalities and sports people due to heart attack despite them being gym attendees . High blood pressure , Diabetes, high cholesterol , Obesity and smoking are the commonly talked about risk factors for heart disease . But unfortunately they account for only about 50% of the deaths . Rest of the risk factors are not routinely assessed .
Our life style plays a major role which is often underestimated by the medical fraternity and public alike . Similarly there are tests which are easily available to diagnose heart disease at their early stages but grossly underused . The preventive cardiology team at PSG hospitals helps to bridge the gaps in preventive care meticulously.,
Prevention is the key which still seems unpopular and under used ..
PEARL CLINIC and HARP, our two keys that are pillared on prevention will provide you with the right solutions to prevent heart disease.
PEARL CLINIC is for primary prevention of diseases ie prevention of heart disease in any vulnerable individuals while HARP guides to prevent progression of disease in patients with established heart disease ie secondary prevention.
PEARL CLINIC is an unique initiative inaugurated on sep 29 th 2021 on the eve of world heart day. PEARL CLINIC derives its name from Prevention and EARLy diagnosis of Cardiovascular and other LIfe style diseases by Novel methods and Integrated and Continued care.
Yes. We focus on all lifestyle diseases and not just Heart disease as all of them are interlinked and are potentially reversible with similar lifestyle changes.
Need for PEARL CLINIC:
Heart disease is the leading cause of death even in covid times, across the globe. Indians have a higher predilection for heart attacks at an early age – at least a decade earlier than their counterparts elsewhere. We tend to have an extensive disease and unfortunately less number conventional risk factors.
Only 50% of those who experience a heart attack have identifiable risk factors.
So our idea is to promote lifestyle changes amongst youngsters by identifying the risk factors and heart disease before they manifest.
Who benefits by PEARL CLINIC?
Anyone who has a risk factor for heart disease – High blood pressure , Diabetes mellitus , obesity , Smoking , high cholesterol , strong family history of heart disease , Sedentary life style ( like IT professionals , Bank staffs ) People with fatty liver , polycystic ovarian disease , erectile dysfunction, History of High blood pressure or sugar during pregnancy , Stress disorders , Transplant patients , Chronic Kidney diseases , dental diseases , certain autoimmune /rheumatological conditions , patients with family history of cancer breast , past history of cancer breast.
What’s done in PEARL CLINIC ?
Assessment
- Anthropometric assessment – BMI, Waist-Hip Ratio and skin fold thickness.
- Evaluation of Physical Activity – Flexibility, Strength, Endurance and Balance.
- Comprehensive Diet Assessment, Food Preferences and Food Economics.
- Established Risk Score Assessment for Diabetes and Heart Disease
Consultation
- Group Consultation with YOGA and Naturopathy Doctor for YOGA and breathing exercises.
- Individual consultation with Dietitian for personalized diet prescription.
- Individual consultation with Physiatrist for tailor-made exercise prescription
- Individual consultation with Cardiologist to get an overview of investigations and for final summary
Continued Care
- Feasible plan of action to attain set goals is arrived with individual’s concurrence.
- Periodic follow up (at two, four and twelve weeks) as per plan of action and further modification of lifestyle changes depending on the individual’s ability to adhere to the original plan
Our Plans for the Near Future
Apart from the services offered above we plan to screen cooking demonstration videos, offer suggestions for kitchen gardens and conduct personalised stress management sessions. What are the investigations done under PEARL CLINIC ?
Basic blood and urine investigations to assess your risk profile which include complete blood count ,blood grouping ,fasting and postprandial blood sugar , glycosylated hemoglobin(HbA1C) ,lipid profile, renal parameters, TSH ,uric acid and microalbuminuria Comprehensive investigations include Homocysteine, hsCRP, Lipoprotein (a), ApoA, Apo B and Small density LDL.
Investigations which detect early changes in the blood vessels are done to look for early disease at which stage we can work on halting the disease process. They include Arterial Pulse Wave Velocity , Endothelial function measurement by ENDOPAT and Detection of coronary calcium .
Cardiopulmonary exercise testing is done to assess the ability of your heart , lung and muscles during exercise. This test helps us to provide you with a better exercise prescription. The Ultrasound of abdomen gives an idea about visceral fat and Polycystic ovarian disease in females.
For details on various PEARL packages please Click Here
HARP – Heart Awareness and Rehabilitation Program is an indoor program to assist patients who already have a heart problem
Need for HARP :
The present day medications and procedures like stenting and bypass surgery provide most often symptomatic benefits and are unquestionably warranted in patients with heart attack, to limit the damage to heart muscles as well as in patients with refractory symptoms. However the basic pathology remains unaltered by these measures . The procedures are not largely to prevent future problems. This calls for major life style changes .
Moreover , the blockages in the heart vessels might recur in the future in the same or a new site and are at times very troublesome . In some patients , second procedure / surgery might be risky or ineffective . Here lifestyle changes are known to play a pivotal role . So should we wait for problems to recur at all ..?!
Who is eligible for HARP?
If you have had
- A Heart attack
- Coronary artery bypass graft (CABG) surgery
- Interventional procedures such as balloon angioplasty, PTCA, or stent placement
- Peripheral artery disease
- Stroke
We encourage all those who have persistent symptoms following heart attack / stroke / bypass surgery or stenting and those who want to avoid symptoms following an attack / stroke/ any cardiac procedure.
The Beginning :
With a focus on improving the quality of life in cardiac patients , the Cardiology Department, PSG hospitals has developed a 7 day program in which symptomatic Heart Disease patients are given supervised dietary intervention and physical exercise. Apart from the routine cardiac investigations, each patient’s endothelial function is also checked. After the intervention for a period of just 7 days, all the patients have shown an improvement in their endothelial function, reduced symptoms like daily chest pain on exertion, drastically improved blood sugar levels and the reduced requirement of medications. Considering how successful and popular the program has been it has been extended to ten days with introduction of group yoga sessions and relaxation methods. This program is just not for patiens with heart disease, but anyone who has focus on promoting good health can join for healthy living and a sense of well being.
Cardiac Rehabilitation Program
We have a full fledged rehabilitation team to take care of patients who are admitted with heart attack ( myocardial infarction ) or heart failure . All in- patients are provided whole food plant based diet , there by making it easy for them the same diet at home post discharge .All in-patients get phase 1 physical rehabilitation . At discharge they are offered different packages (weekly once to thrice week) for phase 2 & phase 3 rehabilitation. Interested patients can enroll themselves for yoga program as well.
Considering the growing burden of heart disease we have extended our services to the community as well. Some our community based interventions include..
Community program for primary and primordial prevention
We have started a community program VRHHRI (V Rajan Heart Health Initiative) in Mallegoundanpalayam- the ancestral village of Late Shri V Rajan , our former trustee as desired and patronized by his family . As an initial step , we have done complete screening of families who came forward for risk factor screening . Our doctor visits the village twice a week to take care of the basic health needs of the people . From 2022 , we intend to take up interested families for primary prevention program with main focus on promoting healthy cooking habits , promoting kitchen garden and physical activity.
School and college screening program
We follow a comprehensive approach for primordial and primary prevention of heart disease in children, adolescents and young adults through our school and college health program. We provide health education services to students, their parents, teachers and also counsel the administrative staff for offering health diet at the canteen, provide more time for physical activity and have facilities in place for early identification of students with psychological problems.
Industry screening
Unhealthy lifestyle among workers are linked to 66 percent increased risk for loss of productivity in industries. The preventive cardiology has extended its support to industries since 2019 for providing preventive health care. Our services include doing basic investigations, consultation with physiatrist, dietitian and doctor for high risk individuals and health education to all workers. We offer to provide support for changing food pattern in the canteens and creating a work place environment conducive to increase physical acitivity and eliminate sedentary lifestyle
Family screening program
We are introducing this small basic package for family members of people who have suffered a heart attack
Women cardiac screening :
In PEARL clinic , we have introduced the gender specific assessment and investigations for early identification risk factors for heart disease
Our Clinical Team
The Preventive Cardiology & Rehabilitation Section includes
- Cardiologist ,
- Preventive care physicians / public health doctor ,
- Nurse and other healthcare professionals from other departments, including:
- Exercise Physiology
- Nutrition Therapy
- Yoga and natural sciences
- Medical social workers
Multidisciplinary treatment strategies with individualized treatment plans with cutting edge risk evaluation are the unique feature of our programs.
State-of-the-art monitoring equipment and a variety of exercise equipment are available for your safety and convenience.
How do I enter the program?
For PEARL clinic appointments, kindly contact our PEARL clinic support desk @ 9894097730, available from Monday to Saturday between 8.00 am to 5.00 pm.
- Non Invasive
- ECG
- ECHOCARDIOGRAM (ADULT,PEADIATRIC,TRANESOPHAGEAL,STRESS ECHO)
- 24 HR HOLTER MONITORING
- 24 HR AMBULATORY BLOOD PRESSURE MONITORING
- TMT
- Head up tilt table test( HUTT)
- TAVR
Comprehensive screening packages
- Hypertension
- DVT/PTE
- Young Myocardial Infarction
- Pulmonary Hypertension
- Heart Failure Work up
- Vasculitis work up
Preventive measures would be done under various modalities
- Consultation with the Cardiologist
- Biochemical risk stratification
- Diet counseling
- Physical exercise counseling
- Rehabilitation for cardiac patients, stress management and yoga.
Interventional Services
- 24 X 7 Primary PCI services for acute cororany syndromes
- Coronary angiogram/angioplasty
- Pericardiocentesis
- Pacemaker implantation (Temporary, Permanent)
- Electrophysiology study and ablation for arrhythmias
- ICD,CRT
- Pediatric interventions- ASD,VSD,PDA device closure,Pulmonary balloon Valvotomy
- Balloon mitral Valvuloplasty for Rheumatic Mitral stenosis
- Cath study for congenital heart disease
We are privileged to say that we have saved many limbs through intraarterial thrombolysis. Our timely intervention has saved many patients from disabling strokes. We are actively involved in many other peripheral interventions which are helpful in reducing morbidity and mortality in critically ill patients.
Following are a list of peripheral procedures routinely being performed in our department.
1) Intra arterial lysis
- Acute limb ischemia
- Acute CVA(intraarterial lysis)
2) Embolisation
- Uterine artery embolisation
- Bronchial artery embolisation
- Visceral arterial embolisation (Renal, splenic, hepatic)
3) Peripheral arterial interventions
- Aortic and other arterial aneurysm requiring endovascular repair
- Aortic and peripheral vascular ( Renal,subclavian,brachial,Iliac,Femoral and below the knee vessels) stenosis requiring angioplasty and stenting
- Aortic and peripheral vascular ( Renal,subclavian,brachial,Iliac,Femoral and below the knee vessels) stenosis requiring angioplasty and stenting
4) Venus interventions
- IVC filter
- Local lysis for DVT
- Hepatic and IVC recanalization in Budd chiari syndrome
- TNChief Minister health insurance scheme.
- ESI
- ECSH
- Pvt Insurance
Specialist Doctors
Super Specialties Departments
- Aesthetic / Cosmetic Surgery
- Bariatric & Metabolic Surgery
- Cardiology & Preventive Cardiology
- Cardiothoracic & Vascular Surgery
- Clinical Hematology
- Critical Care Medicine
- Developmental Pediatrics
- Emergency Medicine
- Endocrinology & Diabetology
- Endo Gynecology
- Family Medicine
- Fertility Clinic & Centre for Reproductive Medicine
- Fetal Medicine
- Gastroenterology
- Genetics
- Geriatric Medicine
- Gynecologic oncology
- Heart & Lung Transplant LEADING IN THE REGION | One of the Best in the Country
- Hepato-Pancreato-Biliary Surgery & Liver Transplant
- Home Health Service
- Immunology
- Interventional Radiology
- Maxilo Facial Surgery
- Medical Oncology
- Naturopathy & Yoga
- Neonatology
- Nephrology
- Neurology
- Neurosurgery
- Nuclear Medicine
- Paediatric Surgery
- Pain Medicine
- Palliative and Hospice Care
- Pediatric Cardiology
- Pediatric Oncology
- Physical Medicine & Rehabilitation
- Plastic Surgery
- Pulmonology
- Radiation Oncology
- Rheumatology
- Robotic Surgery
- Surgical Gastroenterology
- Surgical Oncology
- Urology & Andrology
Find a Doctor!
J S BHUVANESWARAN Department of Cardiology & Preventive Cardiology, PSG Hospitals
| Specialty | Cardiology & Preventive Cardiology |
| Experience | 32 Years |
| Qualification | MBBS, MD, DM |
| Designation | Professor/Director/Sr. Consultant |

RAJENDIRAN G Department of Cardiology & Preventive Cardiology, PSG Hospitals
| Specialty | Cardiology & Preventive Cardiology |
| Experience | 35 Years |
| Qualification | MD, DM(cardio) |
| Designation | Professor/Senior Consultant |

TAMILARASU K Department of Cardiology & Preventive Cardiology, PSG Hospitals
| Specialty | Cardiology & Preventive Cardiology |
| Experience | 20 Years |
| Qualification | MD.,DNB (Cardiology) FACC |
| Designation | Professor/Senior Consultant |

P RAMASAMY Department of Cardiology & Preventive Cardiology, PSG Hospitals
| Specialty | Cardiology & Preventive Cardiology |
| Experience | 40 Years |
| Qualification | MD., DNB (Cardiology) |
| Designation | Professor/Consultant |

VIDHYAKAR BALASUBRAMANIAN Department of Cardiology & Preventive Cardiology, PSG Hospitals
| Specialty | Cardiology & Preventive Cardiology |
| Experience | 19 Years |
| Qualification | M.D, D.M (CARDIOLOGY), FELLOWSHIP IN CARDIAC ELECTROPHYSIOLOGY. |
| Designation | Associate Professor/Consultant |

Minoti Subhash Kale Department of Cardiology & Preventive Cardiology, PSG Hospitals
| Specialty | Cardiology & Preventive Cardiology |
| Experience | 17 Years |
| Qualification | MBBS., DCH., DNB (Paediatrics)., MNAMS., FPC |
| Designation | Consultant |

B GOKHULARAJ Department of Cardiology & Preventive Cardiology, PSG Hospitals
| Specialty | Cardiology & Preventive Cardiology |
| Experience | 1 Years |
| Qualification | MD, DrNB., |
| Designation | Assistant Professor / Consultant |

PREM KRISHNA ANANDAN Department of Cardiology & Preventive Cardiology, PSG Hospitals
| Specialty | Cardiology & Preventive Cardiology |
| Experience | 18 Years |
| Qualification | M.D(Int Med)., MRCP(UK)., DNB(Card)., D.M.,(Card) |
| Designation | Visiting Consultant |

ARUN KAUSHIK PONNUSAMY Department of Cardiology & Preventive Cardiology, PSG Hospitals
| Specialty | Cardiology & Preventive Cardiology |
| Experience | 6 Years |
| Designation | Visiting Consultant |
Request an Appointment
-

Share with us
Click Here -

Organ Transplantation
Click Here
Copyrights © 2025 PSG Hospitals. All Rights Reserved.